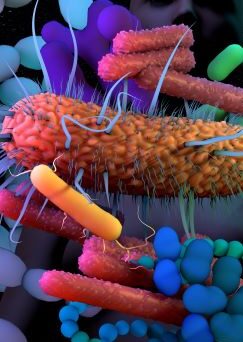
In many senses the true heart and soul of the body is the gut. Yet the gut is so much more than merely an organ. It’s a dynamic, hybrid ecosystem, riven through the very core of us, forming a metabolic interface where two complex biological and chemical worlds – ours and that of the external environment – collide. It occupies a unique position as our metabolic interface with the external world, literally the outside world, inside.
Unsurprisingly, this unique ‘fourth dimension’ of health, formed in that empty space we call the gut, can do almost anything. A biological foundry where other organisms cooperate with our own body cells in complex ways to work magic. Potentially our most powerful sensory organ, the gut is where we feel the deepest of all emotions before our brain can recognise them. It also senses and neutralises threats, the foundation of immunity. It’s a terrain as complex as any environmental ecosystem, that nourishes all body processes, digesting, analysing, processing, and absorbing. It’s the safe space for dumping waste and toxins. It’s even a whole other huge pool of genetic potential, producing many metabolites we’ve evolved to depend upon.
It’s almost a cliché to say the gut is at the centre of health, and probably still too much a simplification. Certainly, there are complex two-way interactions between gut and the rest of the body. As our gut function affects our nervous response, so nervous response impacts gut. As immune function supports the balance of our microbiome, so the microbiome is essential for immunity. And so on…
Is ‘precision medicine’ the right approach to gut health?
Has our thinking about gut health become a bit too compartmentalised? As we learn more about elements of it and test specific aspects of digestion, it can become reduced to a set of functions and parts to be analysed and targeted. But are we still only scratching the surface and is there a danger we might be intervening in complex microbiological relationships we don’t understand? Should we engage in ‘precision intervention’ with the microbiome, or step back and take a more ecological approach?
about elements of it and test specific aspects of digestion, it can become reduced to a set of functions and parts to be analysed and targeted. But are we still only scratching the surface and is there a danger we might be intervening in complex microbiological relationships we don’t understand? Should we engage in ‘precision intervention’ with the microbiome, or step back and take a more ecological approach?
The growth of functional testing in the recent years has been exciting, insightful, and has enhanced our clinical practice; particularly when it comes to stool testing. We can now look at multiple stool markers and through PCR analysis, we can get a good insight into the state of the microbiome. However, when looking at the detail and searching for the root cause of one’s symptoms, do we sometimes unintentionally miss the wood for the trees?
It is sometimes easy and convenient to find that one underlying cause, whether it’s a Candida overgrowth, SIBO, or a parasitic infection, and have a specific protocol to manage it. But is that the holistic approach? Are we assessing the whole person and considering the complex interactions between different body systems?
There is rarely one single ‘root cause’ to health issues. As soon as one part of the system is affected, other parts adapt and compensate. Where does cause start and effect end? Understanding the system dynamics, and its interaction with the wider environment enables us to intervene in multiple ways and facilitates a better state of balance and function.
When we do testing and naturally zoom in on the detail, we need to remember to zoom out. The zooming in should only be for finding out that awkward piece of the puzzle, only to then put it together with other pieces and look at the whole picture.
Zooming in – What are we missing?
With all the great, advanced testing options we have, there are still a lot of unknowns; we don’t fully understand what the right microbiome is for each person, or even the full complexity of how microorganisms behave, and particularly, when they co-exist in that complex and diverse community. An isolated microbe cannot be expected to behave in the same way when it’s surrounded by dozens of other microbes.
Are the ‘baddies’ always bad? Let’s start with Candida albicans… It’s an opportunistic yeast, which, if allowed to proliferate, can contribute to all sorts of problems ranging from IBS-symptoms, to brain fog, and mental health issues. If we go back 10, 15 years, our key approach to dealing with this yeast was to starve it by adopting a strict low sugar and yeast diet. Whether this was following a self-diagnosis, or some form of testing, many people would later find that their symptoms and Candida would eventually come back. Whilst we know sugar is an issue, now we know more about Candida and its behaviour and the fact that it can evolve under favourable conditions. Most individuals have some amount of Candida growing in their gut, but the numbers are kept in check by a robust immune system.1 Compromised immunity, often characterised by low secretory IgA, can lead to Candida evolving into the more aggressive mycelial form, hijacking nutrient supplies (or even switching to non-sugar sources), and establishing more dominance over the beneficial microbiota.1,2,3
 Other studies have highlighted that the very microorganisms that we often try to eliminate with antimicrobials and targeted protocols have actually proven to be a normal part of the microbiome, or even beneficial in some cases. For example, the parasite Blastocystis hominis¸ which is famous for being hard to eradicate, has actually been associated with a reduced risk of GI disease.4 Its elimination through improved hygiene over the years may have removed an important educator of our immune systems.4 There are in fact many different genotypes of this parasite, some pathogenic and some not, so appropriate testing is required to ensure that we’re not treating something that may in fact be a healthy resident of the microbiome.5 There are also examples that emphasise that the microbe itself, when in low to moderate colony size, is not an issue. For example Escherichia coli is a healthy competent of the microbiome and is important for digestion and immune defence,6 in certain scenarios, specific strains of E.coli can overgrow into a state of dysbiosis, yielding negative consequences for the host.7. Similarly, Pseudomonas aeruginosa remains relatively harmless in small amounts, but once its population size reaches a certain threshold, the bacteria can rapidly overwhelm host defences by activating genes that regulate biofilm formation and virulence.8
Other studies have highlighted that the very microorganisms that we often try to eliminate with antimicrobials and targeted protocols have actually proven to be a normal part of the microbiome, or even beneficial in some cases. For example, the parasite Blastocystis hominis¸ which is famous for being hard to eradicate, has actually been associated with a reduced risk of GI disease.4 Its elimination through improved hygiene over the years may have removed an important educator of our immune systems.4 There are in fact many different genotypes of this parasite, some pathogenic and some not, so appropriate testing is required to ensure that we’re not treating something that may in fact be a healthy resident of the microbiome.5 There are also examples that emphasise that the microbe itself, when in low to moderate colony size, is not an issue. For example Escherichia coli is a healthy competent of the microbiome and is important for digestion and immune defence,6 in certain scenarios, specific strains of E.coli can overgrow into a state of dysbiosis, yielding negative consequences for the host.7. Similarly, Pseudomonas aeruginosa remains relatively harmless in small amounts, but once its population size reaches a certain threshold, the bacteria can rapidly overwhelm host defences by activating genes that regulate biofilm formation and virulence.8
An increasingly popular diagnosis these days is SIBO, but does it have real clinical validity, or do we need to consider it is a diagnosis too far, perhaps narrowing our view? Whilst SIBO can very much be a problem for a person, it’s often accompanied by wider digestive dysfunction such as slow motility, colonic dysbiosis, or decreased levels of digestive enzymes. The testing methods and their validity have also been challenged, with false-positive and false-negative results being common.9,10 Is there an element of observer bias, because of the knowledge that SIBO might exist and the test you use? While you are looking for and noticing SIBO, what aren’t you looking for and not noticing?
Unfortunately, in the past, there’s been an exaggerated focus on the overgrowth of microorganisms and an overreliance on antimicrobial supplements, antibiotics, and a low FODMAP diet, without addressing the wider digestive dysfunction.
Yet, all is not lost; more and more experts and practitioners are highlighting the need for working on the whole GI tract. I particularly liked a comment from a practitioner on one of the popular social forums: “SIBO is not an infection, it’s an imbalance of the gut ecosystem”.
Zooming out – Taking an ecological approach to gut health
The gut is an interlinked system of multiple organs, tissues, and microbiota, working together to digest, absorb nutrients, excrete toxins, provide immune protection, and acting as a physical barrier. As we’ve seen in the examples above, very often it is not about that single cause or microorganism, but it’s about the internal environment that is somehow dysfunctional, allowing the microbe to replicate, evolve, and sometimes take over.
Nurturing a diverse microbiome is a good starting point and using pre-and probiotics is in most cases beneficial. The impact of a good probiotic combination is to positively alter the gut habitat through competition, immune stimulation, and secretion of naturally regulating substances. In fact, certain probiotics can really help with SIBO, because they have an overall effect on rebalancing gut flora.11,12 While avoiding fibre may be necessary in a severely compromised gut, it can lead to greater fibre intolerance and further dysbiosis.13 There might be an argument to sometimes be careful about the levels of prebiotics, but in general the goal should always be to get people to tolerate a high soluble fibre diet, containing a breadth of different prebiotics.
Appropriate digestion of foods with adequate levels of hydrochloric acid, enzymes, and bile, ensures there is less food for pathogenic organism, better host nutrition status, and less immune reactivity. Unabsorbed protein is fermented by bacteria capable of proteolysis, resulting in high ammonia and branched chain fatty acids (BCFAs).1 In addition, good motility and a well-functioning Migrating Motor Complex (MMC) are essential to digestion, absorption, integrity, and microbial balance. Disordered motility or diverticulitis14, 2 can further drive an overgrowth of abnormal bacteria, and contribute to SIBO.15,16
And lastly, appropriate integrity of the epithelial tissue characterised by robust connective tissue and adequate mucus,17,18 is paramount for bacterial colonisation and survival, thus promoting microbial balance, appropriate digestion through enzyme secretion by the epithelium, and a strong immune response in case of pathogenic invasion.
We should aim to shift our mindset towards creating the right gut habitat for our individual microbiome to thrive in. In essence, there’s much that we don’t know about the specifics of the gut ecosystem, and, while we should always be interested in specific details and mechanisms, we must also zoom out as well and consider the interconnections between organs and mechanisms, even beyond the gut, rather than restricting our thinking to what is, in essence, an allopathic diagnosis.
At BioCare, we’ve always believed that to truly transform health, we need to use a whole gut, whole health approach. Seeing the gut from an ecological perspective enables us to use our adaptive approach to develop synergistic products that really work, as well as providing unique, free education events to support you. We’ve got some great new innovations right now and coming up this Autumn, like our brand new probiotic products that support specific microbiome needs for female and baby health. If you’re a holistic practitioner, we’d love you to join us in person for our ‘Gut Unravelled’ seminar. We’re working with you, to help you support the Whole in everyone’s Soul!

Bibliography
1. McGuckin MA, Lindén SK, Sutton P, Florin TH. Mucin dynamics and enteric pathogens. Nature reviews Microbiology. 2011;9(4):265-278. doi:10.1038/NRMICRO2538
2. Brown AJP, Budge S, Kaloriti D, et al. Stress adaptation in a pathogenic fungus. The Journal of experimental biology. 2014;217(Pt 1):144-155. doi:10.1242/JEB.088930
3. Berman J, Sudbery PE. Candida Albicans: a molecular revolution built on lessons from budding yeast. Nature reviews Genetics. 2002;3(12):918-930. doi:10.1038/NRG948
4. Loke P, Lim YAL. Helminths and the microbiota: parts of the hygiene hypothesis. Parasite immunology. 2015;37(6):314. doi:10.1111/PIM.12193
5. Tan KSW. New Insights on Classification, Identification, and Clinical Relevance of Blastocystis spp. Clinical Microbiology Reviews. 2008;21(4):639. doi:10.1128/CMR.00022-08
6. (PDF) Reid G, Howard J, Gan BS.. Can bacterial interference prevent infection? Trends Microbiol 9: 424-428. Accessed March 7, 2022. https://www.researchgate.net/publication/11795108_Reid_G_Howard_J_Gan_BS_Can_bacterial_interference_prevent_infection_Trends_Microbiol_9_424-428
7. Ormsby MJ, Logan M, Johnson SA, et al. Inflammation associated ethanolamine facilitates infection by Crohn’s disease-linked adherent-invasive Escherichia coli. EBioMedicine. 2019;43:325-332. doi:10.1016/J.EBIOM.2019.03.071/ATTACHMENT/EE26E89C-52C7-4FD3-A8B1-D2E6965EAF94/MMC1.PDF
8. Miller MB, Bassler BL. Quorum Sensing in Bacteria. http://dx.doi.org/101146/annurev.micro551165. 2003;55:165-199. doi:10.1146/ANNUREV.MICRO.55.1.165
9. Bures J, Cyrany J, Kohoutova D, et al. Small intestinal bacterial overgrowth syndrome. World Journal of Gastroenterology : WJG. 2010;16(24):2978. doi:10.3748/WJG.V16.I24.2978
10. Yao CK, Tuck CJ. The clinical value of breath hydrogen testing. Journal of gastroenterology and hepatology. 2017;32 Suppl 1:20-22. doi:10.1111/JGH.13689
11. Rosania R, Giorgio F, Principi M, et al. Effect of probiotic or prebiotic supplementation on antibiotic therapy in the small intestinal bacterial overgrowth: a comparative evaluation. Current clinical pharmacology. 2013;8(2):169-172. doi:10.2174/15748847113089990048
12. Posserud I, Stotzer PO, Björnsson ES, Abrahamsson H, Simrén M. Small intestinal bacterial overgrowth in patients with irritable bowel syndrome. Gut. 2007;56(6):802-808. doi:10.1136/GUT.2006.108712
13. Huaman JW, Mego M, Manichanh C, et al. Effects of Prebiotics vs a Diet Low in FODMAPs in Patients With Functional Gut Disorders. Gastroenterology. 2018;155(4):1004-1007. doi:10.1053/J.GASTRO.2018.06.045
14. Tursi A, Brandimarte G, Giorgetti GM, Elisei W. Assessment of small intestinal bacterial overgrowth in uncomplicated acute diverticulitis of the colon. World Journal of Gastroenterology : WJG. 2005;11(18):2773. doi:10.3748/WJG.V11.I18.2773
15. Deloose E, Janssen P, Depoortere I, Tack J. The migrating motor complex: control mechanisms and its role in health and disease. Nature reviews Gastroenterology & hepatology. 2012;9(5):271-285. doi:10.1038/NRGASTRO.2012.57
16. Roland BC, Ciarleglio MM, Clarke JO, et al. Low ileocecal valve pressure is significantly associated with small intestinal bacterial overgrowth (SIBO). Digestive diseases and sciences. 2014;59(6):1269-1277. doi:10.1007/S10620-014-3166-7
17. Wacklin P, Mäkivuokko H, Alakulppi N, et al. Secretor genotype (FUT2 gene) is strongly associated with the composition of Bifidobacteria in the human intestine. PloS one. 2011;6(5). doi:10.1371/JOURNAL.PONE.0020113
18. Juge N. Microbial adhesins to gastrointestinal mucus. Trends in microbiology. 2012;20(1):30-39. doi:10.1016/J.TIM.2011.10.001










